Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Tuberculous Mediastinitis with Mediastinal Abscess in an Immunocompetent Man Presented with Fever, Acute Dyspnoea, Chest Pain, Chest Wall Swelling, Acute Kidney Injury, Transaminitis and DIC: Rare Case Report
*Corresponding author: Khin Phyu Pyar, Professor and Head/Senior Consultant Physician, Department of Medicine/ Department of Nephrology, Defence Services Medical Academy, No. (1) Defence Services General Hospital (1000-Bedded), Yangon, Myanmar.
Received: December 06, 2023; Published: December 11, 2023
DOI: 10.34297/AJBSR.2023.20.002763
Abstract
A 45-years-old immunocompetent man had abscess in right side of neck. It was complicated by mediastinitis and mediastinal abscess, acute kidney injury, transaminitis and DIC. CT neck and chest revealed features of mediastinitis and mediastinal abscess in continuation with right cervical lymphadenopathy and abscess. PCR for Mycobacterium tuberculosis was positive in pus drained from anterior mediastinum. We reported a rare manifestation of tuberculous mediastinitis and mediastinal abscess.
Keywords: Cervical lymphadenopathy, Mediastinitis, Mediastinal abscess, Mycobacterium tuberculosis
Introduction
Tuberculosis is one of the top killing diseases particularly in the developing countries. It is caused by Mycobacterium tuberculosis. Lungs are most commonly affected; lymph node involvement is less common. Clinical awareness on tuberculous infection is important if it involves rare site like extra-pulmonary lesion; furthermore, it makes diagnostic challenges if the clinical presentation is not typi cal [1-3]. Among extra-pulmonary lesions, mediastinal tuberculosis is relatively rare [4].
Acute mediastinitis is one of the life-threatening situations requiring early diagnosis and treatment. Clinical manifestations are swelling of chest with tenderness, dyspnoea, cough and fever. Differentiation of cellulitis of chest wall from mediastinitis is not easy if there is no facility for CT scan. Acute kidney injury, transaminitis and DIC are well documented complications in patients with sepsis; however, they are very rarely reported as presentation of tuberculosis [5,6]. Acute kidney injury and transaminitis were reported as side effects of anti-tubercular therapy [7,8].
Case Presentation
The patient was 45-years-old non-immunodeficient man; he developed one week history of fever and painful swelling on right side of the neck. He was previously healthy. The primary physician thought it was pyogenic abscess; and, he performed incision and drainage. Local wound responded well to daily dressing and oral antibiotics, amoxicillin-clavulanic acid. One week later, he noticed swelling over left anterior chest wall. It was shortly followed by high fever, aching chest pain and dyspnoea. Therefore, he was sent to tertiary hospital. He was dyspnoeic; temperature was 103*F; respiratory rate was 24/minute; Sa O2 was 94% with oxygen 2L/minute; pulse rate was 120/minute; blood pressure was 90/50mmHg; tinge of jaundice, feature of inflammation over anterior chest wall was noted. Urine output was 200cc/24hours. There were several areas of ecchymosis over left arm suggestive of Disseminated Intravascular Coagulation (DIC) (Figure 1).
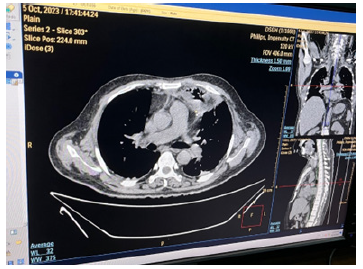
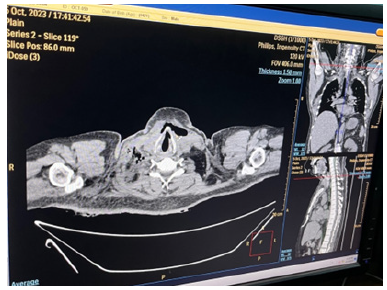
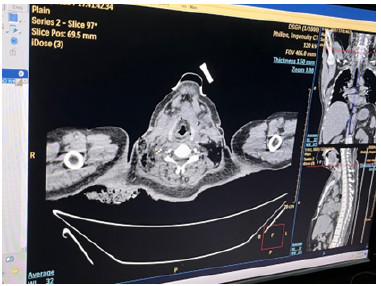
Chest radiograph showed slight widening of mediastinum. Blood for hemoglobin was 11.2gm%; total WBC count was 9.9 X109 /L (Neutrophils 88.1%, Lymphocyte 9.5%, Monocyte 2.4%); platelet count was 36 X109/L; ESR was 40mm per 1sthour; serum creatinine was 4.9mg/dl (0-1.3mg/dl); blood urea was 244.3mg/ dl (10-50mg/dl); serum sodium was 132 ; potassium was 4.4; chloride was 98; total bilirubin was 15.6 mg/dl (0.2-1.0mg/dl); Aspartate aminotransferase was 65U/L (9-48U/L); LDH was 502U/L (200-480U/L). Blood sugar (105.6mg%) and Hb A1 C were normal. Blood for retroviral serology was negative; serology for hepatitis B and C were negative. Computed tomography (CT) neck showed right cervical lymphadenopathy with some areas of break down suggestive of abscess. CT chest revealed features of mediastinitis and mediastinal abscess; they were in continuation with pre-tracheal fascia as seen in CT neck findings (Figures 2-12).
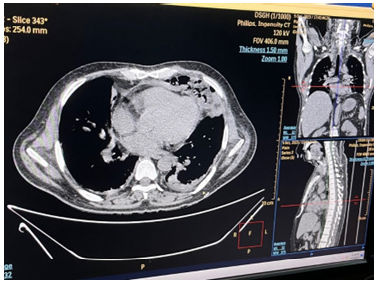
Figure 5: CT chest showing multiple abscess with surrounding opacities in the anterior mediastinum suggestive of mediastinitis and mediastinal abscess, and minimal left pleural effusion.

Figure 6: CT chest showing larger abscess in the anterior mediastinum with minimal left pleural effusion.

Figure 7: CT chest showing larger abscess with surrounding inflammation in the anterior mediastinum with minimal left pleural effusion.
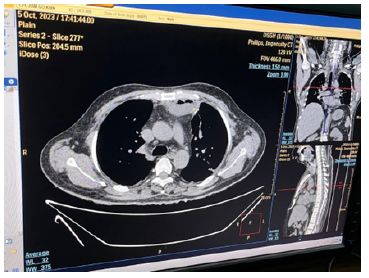
Figure 9: CT chest showing mediastinitis and rounded opacity with air speck at the level of trachea bifurcation.
Therefore, it was percutaneously drained via CT guidance. Figure 3 Brownish pus 100 cc was drained. Figure 4 Thrombocytopenia was corrected with platelet rich plasma. Parenteral antibiotics (Meropenem and Levofloxacin) and fluid replacement were given; total 5 sessions of hemodialysis were done for acute kidney injury. And, the patient recovered gradually. Fever subsided; dyspnoea improved; urine output increased; serum creatine decreased gradually; platelet count became normal. Acid Fast Bacilli (AFB) in Ziehl-Nelson stain of pus drained from mediastinum was negative; however, PCR test for Mycobacterium tuberculosis was positive. Therefore, anti-tubercular therapy (isoniazid, rifampicin, ethambutol and pyrazinamide) was initiated.
Institutional Conflict
Mediastinal tuberculosis is a rare infection resulting from direct inoculation of organisms or through hematogenous spread. Mediastinal abscess due to tuberculosis was reported from rich countries as well as from poor countries [2]. Mediastinal tuberculosis may present as tumour [9]. In this case, the patient presented with swelling of chest with tenderness, dyspnoea, cough and fever suggestive of acute mediastinitis. Acute mediastinitis is one of the life-threatening situations requiring early diagnosis and treatment; the mortality rate is high (40%). Differentiation of cellulitis of chest wall from mediastinitis is not easy if there is no facility for CT scan. It is one reasons for reporting this case.
Regarding the interval between the diagnosis of right cervical abscess and mediastinal abscess, it was 2 weeks in this case. The interval was 4 months in one case report; he was 62-year-old man presented with increasing mass in right mediastinum [10]. Infected lymph nodes may also transfer the bacilli through lymphatic route. In this case, the bacilli from infected right cervical node probably drained to anterior mediastinum through pre-tracheal fascia. Not only cervical tuberculosis but also mediastinal tuberculosis may resemble a pyogenic abscess or tumour [4]. Therefore, it is a clinical challenge for treating physician.
Mediastinal abscess may be complication of surgery or procedure [11,12]. History in this case highlighted the possible association or same etiology; neck abscess and mediastinal abscess. In view of clinical presentation, this patient had acute kidney injury, transaminitis and DIC on arrival to our hospital. Acute kidney injury may result from analgesics, dehydration, septicemia and antibiotics. It recovered with several sessions of hemodialysis, fluids and electrolytes therapy. Having DIC in this case can be explained by septicemia though it is uncommon in tuberculosis. They were very rare manifestation of mediastinal tuberculosis. This is another reason for case reporting.
In low resource setting, finding Acid Fast Bacilli (AFB) in Ziehl- Nelson stain done in sputum smear is not difficult and it is done routinely. In this patient, AFB was not seen in the pus drained from mediastinal abscess possibly owing to paucibacillary load; however, PCR test for Mycobacterium tuberculosis was detected. It supported the fact that PCR for Mycobacterium tuberculosis was a good tool for diagnosis of not only pulmonary tuberculosis Amin et al., (2011) but also extrapulmonary tuberculosis [13-16]. In our country, PCR for Mycobacterium tuberculosis is not easily available in all areas. Therefore, clinical acumen, relative lymphopenia in full blood count and high ESR are good clues to the diagnosis of tuberculosis particularly extra-pulmonary tuberculosis. We would like to highlight the importance of lymphopenia in diagnosing tuberculosis in developing countries.
Conclusion
Clinical awareness on tuberculous infection is important particularly in high tuberculosis prevalence areas. Good clinical acumen and relative lymphopenia in full blood count strongly favor the diagnosis of tuberculosis. Mediastinal tuberculosis (mediastinal abscess and mediastinitis) is uncommon form of extrapulmonary tuberculosis. It should be considered in both immunocompetent and immunocompromised patients. PCR test for Mycobacterium tuberculosis is better than finding Acid Fast Bacilli (AFB) in Ziehl-Nelson stain particularly in specimen rather than sputum.
Ethical Approval
Our institution does not require ethical approval for reporting cases.
Funding
The authors received no financial support for publication of this article.
Informed Consent
The informed consent for publication in this article was obtained from patient.
Acknowledgements
The authors would like to thank the patient for giving consent to this article. Also, to all doctors and nursing team for making great efforts in caring him. The authors acknowledged Professor Ohmar Hlaing for radiological support, Professor Tin Moe Mya for laboratory support, Dr Wah Wah Aung for molecular study, Professor Thet Naing, Professor Myint Zaw, Professor Kyaw Zay Ya and Professor Ko Ko Lwin for administrative support.
Declaration Of Conflict of Interest
The authors declared no potential conflicts of interests with respect to authorship and publication of this article.
References
- Gupta RK, Sharma BK, Jena A, Pant K, Prakash R, et al. (1989) Primary mediastinal tuberculous abscess: Demonstration with MR. Pediatr Radiol 19(5): 330-332.
- Naha K, Vivek G, Padmakumar R, Kansal N, Mk Gupta, et al. (2012) Tuberculous mediastinal abscess as a paradoxical reaction in an immunocompetent individual. BMJ Case Reports.
- Bringmans T, Vanreusel I, Coquilhat A, Derwa S, Van Ierssel SH, et al. (2020) The Diagnostic Challenge of Extrapulmonary Tuberculosis: Esophageal Perforation, Mediastinitis, Pneumopericardium, and Pericardial Abscess Formation. JACC Case Rep 2(2): 266-270.
- Ren X, Li K, Li L, Zhao G (2021) Mediastinal tuberculous lymphadenitis presenting with insidious back pain in a male adult: A case report and review of the literature. J Int Med Res 49(1): 0300060520987102.
- Peerapornratana S, Manrique Caballero CL, Gómez H, Kellum JA (2019) Acute kidney injury from sepsis: Current concepts, epidemiology, pathophysiology, prevention and treatment. Kidney Int 96(5): 1083-1099.
- Campos P, Mano D, Antunes R (2022) Tuberculosis Presenting as Acute Sepsis and Secondary Hemophagocytic Lymphohistiocytosis. Eur J Case Rep Intern Med 9(2): 003121.
- Ata F, Magboul HMB, Toba HAA, Alfar H, Al Bozom A, et al. (2022) Rifampin-induced acute kidney injury and hemolysis: A case report and literature review of a rare condition. Clin Case Rep 10(12): e6780.
- Chang CH, Chang LY, Ko JC, Wen YF, Chang CJ, et al. (2023) Incidence of and Risk Factors for Acute Kidney Injury During Antituberculosis Treatment: A Prospective Cohort Study and Literature Review. Infect Dis Ther 12(3): 919-931.
- Maguire S, Chotirmall SH, Parihar V, Cormican L, Ryan C, et al. (2016) Isolated anterior mediastinal tuberculosis in an immunocompetent patient. BMC Pulm Med 16(1): 24.
- Matsumoto A, Soma T, Shoji T, Katakura H (2022) Mediastinal tuberculosis following descending necrotizing mediastinitis: A case report. Respirol Case Rep 10(6): e0957.
- Zhang H, Geng Y, Zheng Y, Wang Y (2016) A case of anterior mediastinitis and bilateral multiple lung abscesses occurring after trans-subxiphoid video-assisted thoracoscopic extended thymectomy for thymoma with myasthenia gravis. J Thorac Dis 8(9): E970-E973.
- Bispo M, Marques S, De Campos ST, Rio Tinto R, Fidalgo P, et al. (2022) Mediastinal Abscess Formation after EUS-Guided Sampling in a Young Patient with Sarcoidosis: Be Aware of the Increased Risk! GE Port J Gastroenterol 30(Suppl 2): 17-20.
- Amin I, Idrees M, Awan Z, Shahid M, Afzal S, et al. (2011) PCR could be a method of choice for identification of both pulmonary and extra-pulmonary tuberculosis. BMC Res Notes 4(1): 332.
- Honoré Bouakline S, Vincensini JP, Giacuzzo V, Lagrange PH, Herrmann JL (2003) Rapid diagnosis of extrapulmonary tuberculosis by PCR: impact of sample preparation and DNA extraction. J Clin Microbiol 41(6): 2323-2329.
- Mehta PK, Raj A, Singh N, Khuller GK (2012) Diagnosis of extrapulmonary tuberculosis by PCR. FEMS Immunol Med Microbiol 66(1): 20-36.
- Ajantha GS, Shetty PC, Kulkarni RD, Biradar U (2013) PCR as a diagnostic tool for extra-pulmonary tuberculosis. J Clin Diagn Res 7(6): 1012-1015.








 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.